GM case with sob and pain abdomen
A 64 YR M WITH SOB AND PAIN ABDOMEN
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan. is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
A 64 years old male patient barber by occupation came to casuality with chief complaints of shortness of breath and pain in abdomen
History of presenting illness::
Patient was apparently asymptomatic 1 month back and then he developed shortness of breath incidious onset and gradually progressive
No c/o chest pain,Palpations
C/o fever for 3-4days ,high grade, evening rise of temperature associated with chills and rigor
Since one month patient complaints of breathlessness (grade 3) insidious in onset gradually progressive aggrevated on walking and no seasonal variation.
Past History::
Decreased urine output since 6 months
c/o pain abdomen on left lumbar region since 1 week
patient is a known case of HTN since 10 years for which he is on medication (olmosetron tab)
Not a known case of DM,TB,ASTHMA
Personal history:
Apettite-decreased
Diet- mixed
Bladder- decreased
Bowel -abnormal
Family history:
No significant
Treatment
Renal stenting has done
General examination::
Patient is conscious,cohorent , cooperative well known with time, place, person
He is well built and moderately nourish
No pallor
No Lymphadenopathy
No pedal oedema
No icterus cyanosis, clubbing.
VITALS :
Temp : 98.9
Pulse rate-117
Blood pressure :120/70mmhg
Respiratory rate :20 cpm
Spo2 : 90%
SYSTEMIC EXAMINATION:
Respiratory system:
Inspection: chest shape normal,
Breath sounds -vesicular
Dyspnea: present
Palpation: trachea -central
MANAGEMENT :
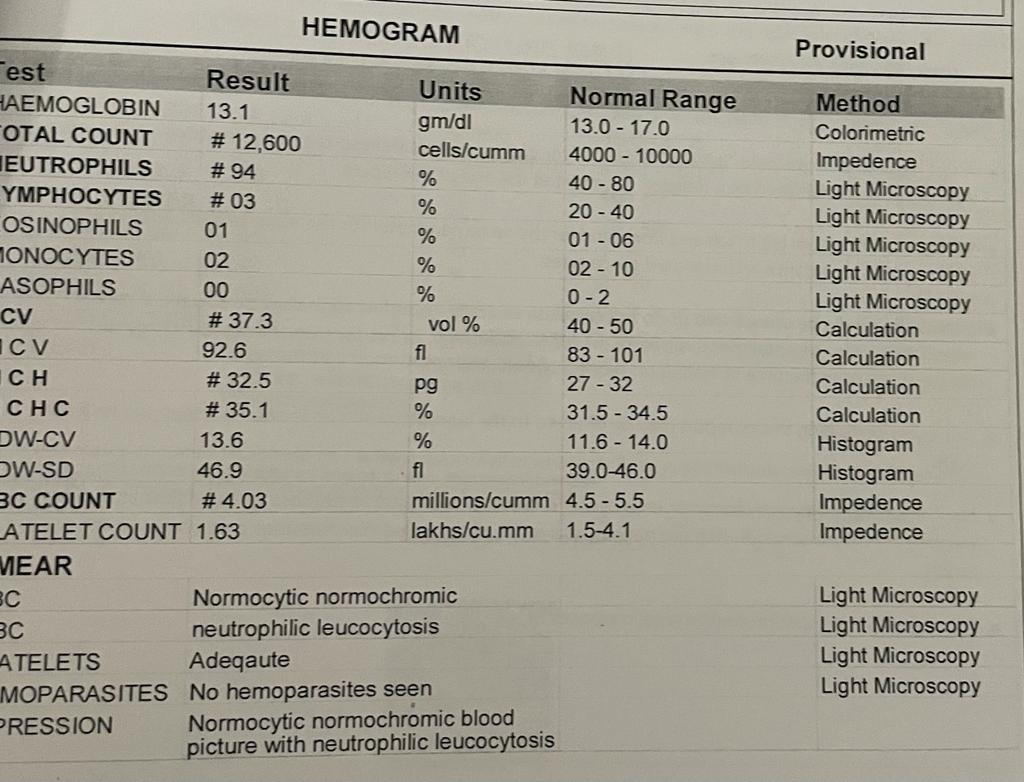
INVESTIGATIONS :






Comments
Post a Comment